The case for adding fluvoxamine to the NIH COVID Guidelines
We don't know why the NIH panel is ignoring fluvoxamine and we aren't allowed to find out.
The biggest lever we have to save hundreds of thousands of lives over the next few months is fluvoxamine. But it isn't even mentioned anywhere in the NIH COVID guidelines. Why? We don't know and we aren't to find out because all the deliberations are secret.
The NIH COVID guidelines committee consists of unpaid, volunteer committee of busy clinicians with no full time administrative staff.
Some NIH committee members participated in the Jan 22, 2021 key opinion leader (KOL) meeting discussing fluvoxamine. But now, more than a month later (Feb 28, 2021), it's pretty clear that they aren't going to mention it in the guidelines. The reasoning is likely this: because there are no phase 3 studies available yet, fluvoxamine is simply lumped in with hundreds of drugs being investigated. They basically don't look at it until you have phase 3 data. It's the same criteria that leading academic hospitals use: no phase 3 data, no evaluation. We don't care how good your data is that is on the table; we have a reputation to maintain and we can't take any chances of being wrong since that would hurt our credibility in the future.
But that's a really bad criteria in a pandemic where there are no approved outpatient treatments that are generally available. The NIH should review the top 5 most promising drugs and make a determination on each of them. And there is absolutely no question that fluvoxamine is in the top 5, and I would argue is at the very top of the list. It's the only drug where a KOL panel has met and voted more than 2:1 in support of the drug.
Here is a summary of why fluvoxamine should be considered by the committee for shared decision making.
We knew from November 12, 2020 with the publication of the Lenze study in JAMA it was a potential game changer because the effect size on reducing hospitalization was 100% and the the supporting data (multiple observational studies) was all consistent. Just two weeks later, on December 1, 2020, we knew that the study was confirmed in a real-world evidence trial by Dr. David Seftel at the massive COVID outbreak at Golden Gate Fields.
Efficacy
As of today (Feb 3, 2021), all of the data I'm aware of is all positive: we learned from the Seftel study that everyone who takes the drug has their symptoms resolve in a few days if we catch them early enough. But we have anecdotal evidence that fluvoxamine works in other stages of the disease.... I've never heard of a case where any person failed to respond and get back to normal no matter how sick they are... high flow oxygen, intubated patients, etc. It just takes longer and may require a larger dose.
An average effect size of 100% prevention of both hospitalization and long term COVID symptoms after two weeks vs. 12.5% (hospitalization rate) and 60% (long-term COVID symptoms rate) respectively for no treatment in the Seftel study. The combined p-value of just the Lenze and Seftel studies is <.0001. While you can argue that you can't combine the numbers because the Seftel study was only pseudo randomized and open label, if you look at the Seftel study, the treatment cohort was worse than random based on comorbidities (add in the fact that it included 8 crossovers from the treatment group (who were not counted twice). Therefore the p-values and effect sizes are thus conservative estimates rather than optimistic estimates. The Fisher Exact test shows an effect size of 75% or more with 95% confidence.
All of the observational studies (two French, one German, and one US) showed significant protection with strong p-values.
Safety
As far as I know, there is no data anywhere showing fluvoxamine would cause a single additional death (it will not make COVID outcomes worse). It is safe drug with no reported deaths of overdose in the literature, making it far safer than over the counter drugs such as Tylenol which kills hundreds of people per year. We know the short and long-term safety outcomes when used with COVID: there are no issues. Mild nausea was reported by one patient on the 50mg BID dose.
Other considerations
Fluvoxamine is a cheap drug, available now, it can be produced in high volume, it has a 37 year safety record, we can ramp up production almost instantly to very high volumes.
Evidence quality
The guidelines committee considers all evidence in their decision. For example, poor quality evidence was used to justify a neutral position on Ivermectin.
This means the guidelines committee is permitted to include all the compelling observational studies that confirm fluvoxamine's effectiveness as well as the RCT and RWE.
We have a great deal of evidence that fluvoxamine is safe and effective. The fluvoxamine data is in a public repository.
Independent expert opinion
We know the KOL meeting (with NIH, CDC, and academic experts) reviewed the two studies and the mechanisms of action and voted overwhelming in favor of shared decision making by more than a 2 to 1 margin (voting 11 in support to 5 opposed). It took just a little more than an hour.
Calculations of lives that could be saved
Today, any calculations for the likely lives saved from this generic drug are hidden from public view (per the rules of the committee), yet this is of great public interest and benefit. A conservative estimate would be roughly 75,000 lives per month if we take the worst case effect size.
Priority
Fluvoxamine should rise to the very top of the agenda since it has the largest potential impact on lives saved. Sadly, we have no idea where it is on the committee's priority list.
Lack of action
So why is there no action from the committee when thousands of people die a day? Why not follow the KOL advice to support shared decision making now and you can refine the recommendations later?
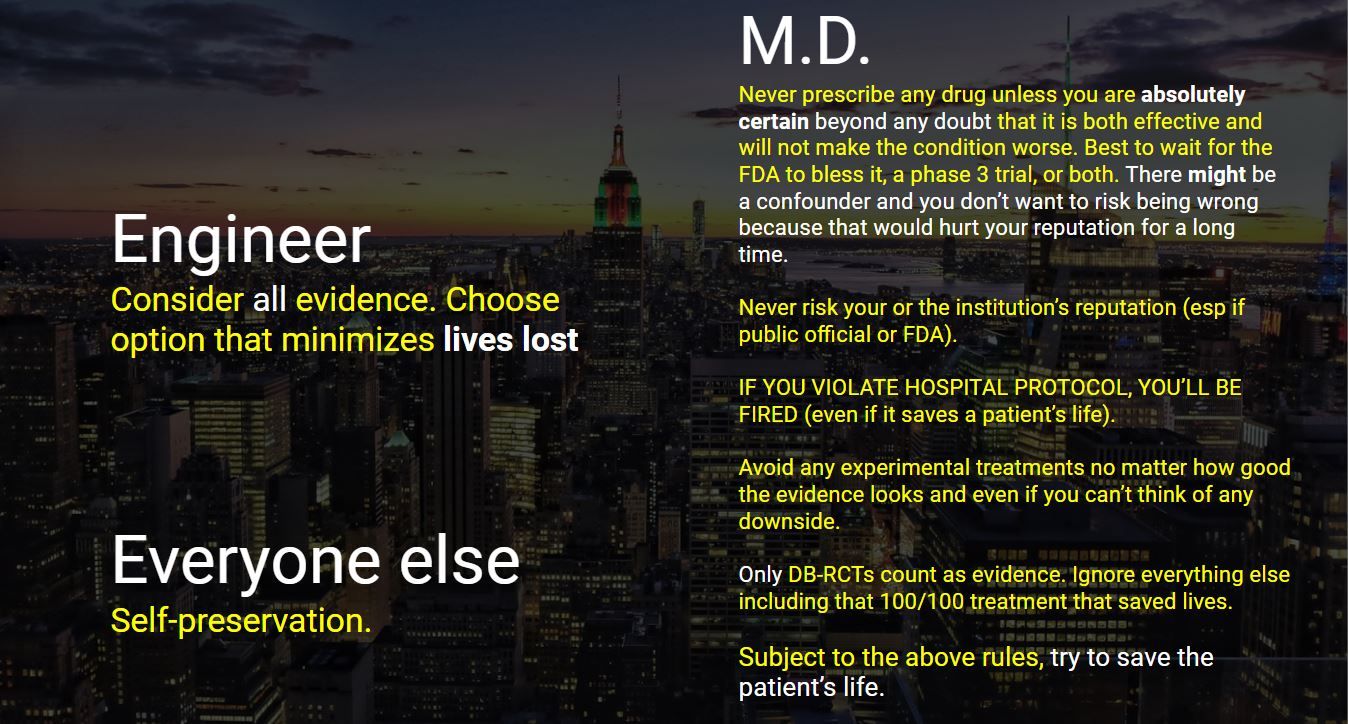
Answer: it's safer and easier just to wait for the phase 3 data. It would be an entirely different story if the NIH panel members themselves had COVID. Then their life would be at risk. But what's at risk for the NIH panel members is their reputations. So conservatism rules the day. They are clearly not in it to maximize the number of lives saved, because if they were, they'd be all over this.
This is highlighted in this graphic which explains the different decision making processes:
Rule changes
Wouldn't it be great if the FDA had to provide a preliminary assessment of an EUA application within 72 hours upon application? It would save so much time. We filed over 4 weeks ago and have gotten zero feedback from the FDA other than the name of the organization processing our request and that it will take more than 5 weeks to provide any feedback whatsoever.
This would require a rule change that Congress would have to instigate, but there is apparently no appetite for this. The process is so perfect now that Congress is afraid of touching it.
Who is accountable?
Thousands of people are dying every day. It took an expert committee a little over 1 hour to make a determination. Why is the guidelines committee taking so long with so many lives at stake? They could be couching their recommendation as "based on the evidence on the table today and the urgency of saving lives, we are recommending this as the most likely outcome of our deliberations, while we further study the data."
It is not the virus that can be blamed for COVID deaths any more. The focus now shifts to the FDA and the NIH Guidelines committee members as well as those empowered to change the rules to enable transparency and expediency, yet decline to do so.